Effective Ways to Optimize Your Gastroparesis Diet for Better Digestion in 2025
Managing a gastroparesis diet effectively is crucial for improving digestive health and overall well-being. This condition affects stomach motility, making it essential to adopt specific **gastroparesis food choices** that support digestion and alleviate symptoms. This article will guide you through many effective strategies, covering everything from meal planning to calorie-rich snacks. As we explore each area, you’ll find that optimizing your diet doesn’t just enhance digestion – it also plays a significant role in maintaining your energy levels and nutritional balance.
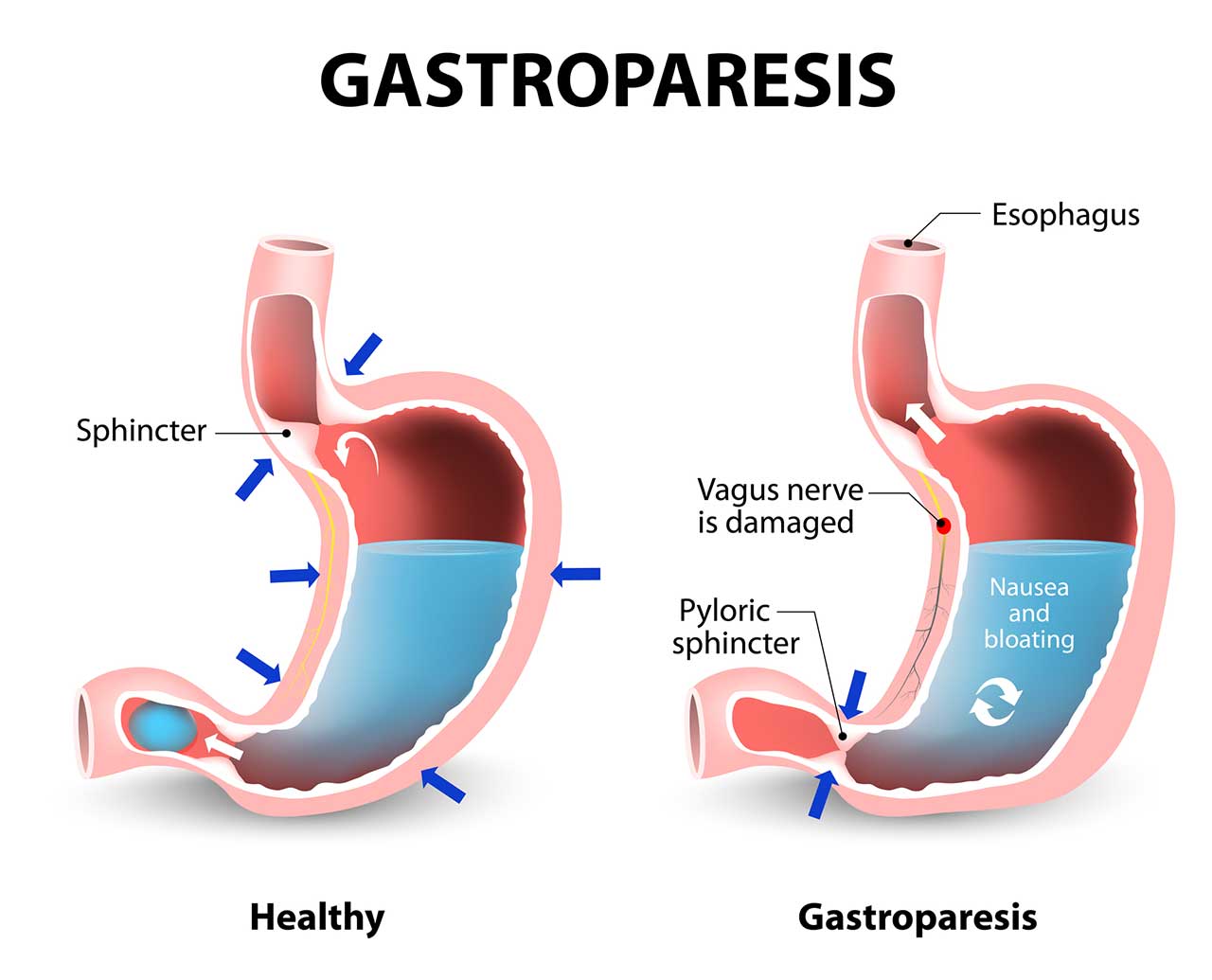
Understanding Gastroparesis and Its Dietary Implications
Gastroparesis is a condition characterized by delayed stomach emptying, leading to various digestive issues such as bloating, nausea, and abdominal pain. Understanding **how food choices** impact gastroparesis is vital. The condition’s management requires adhering to a diet that often involves **small frequent meals** tailored to individual dietary needs, helping to mitigate symptoms and ensure proper nutrient absorption. Factors such as **nutritional value**, tolerance to certain ingredients, and cooking methods can significantly influence your dietary experience and digestive health.
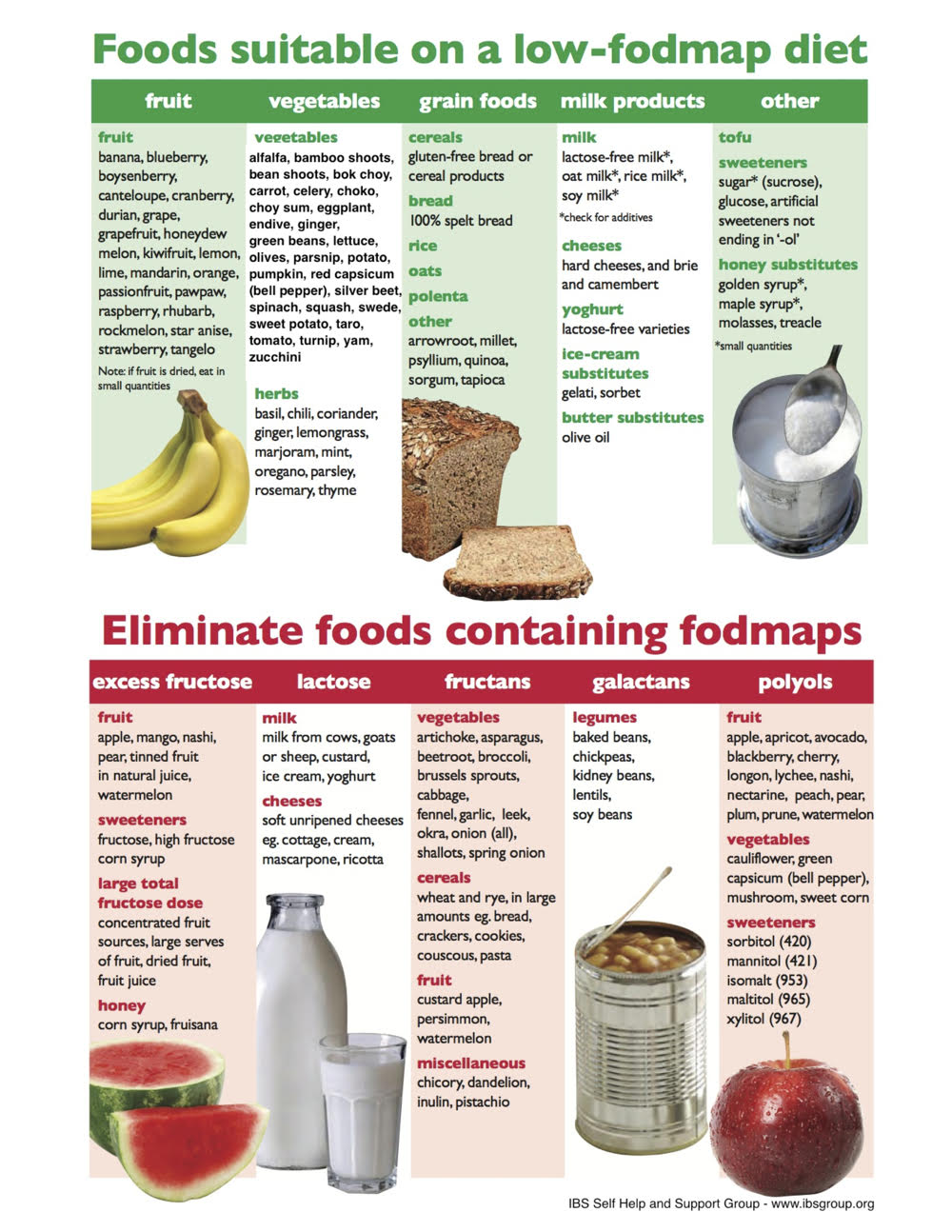
Key Dietary Restrictions for Gastroparesis
When it comes to managing your gastroparesis diet, certain dietary restrictions play a crucial role. Foods that are high in fat and fiber can exacerbate symptoms by delaying stomach emptying, so it is beneficial to focus on a **low-fat diet** consisting of **soft foods for gastroparesis** that are easier to digest. Avoiding carbonated beverages and choosing bland and low residue diet options can also contribute to a smoother digestive process. At the same time, keep an eye on **foods to avoid**, such as raw vegetables and high-fiber fruits, which can lead to discomfort.
Identifying Safe Food Options
Finding **safe foods for gastroparesis** is a crucial aspect of dietary management. Generally, lean proteins such as chicken and fish, alongside easily digestible carbohydrates, are excellent choices. Incorporating **high-calorie meals** like nutrient-dense smoothies or **meal replacement shakes** can help achieve calorie goals without adding to digestive strain. Selecting foods based on **nutrition facts** and steering clear of troublesome ingredients will help you create a tailored nutrition plan that promotes effective digestion and overall health.
Importance of Portion Control and Meal Timing
When managing gastroparesis, **portion control** is essential, as large meals can be overwhelming for a sensitive digestive system. Adopting strategies like **meal frequency**—having multiple smaller meals throughout the day—can lead to better symptom management. Utilizing meal planning apps to help schedule your eating and staying mindful of your eating habits can vastly improve your relationship with food. Make sure to establish a regular eating schedule that aligns with your lifestyle; plan for meals out and practice **meal timing strategies** to maximize your dining experiences.
Meal Planning and Preparation Techniques
Successful **gastroparesis meal planning** hinges on understanding your dietary preferences and restrictions. Developing a personalized meal plan that incorporates a variety of **easy-to-digest foods** is vital for maintaining energy levels while managing symptoms. Take note of helpful **cooking techniques for gastroparesis**, such as gentle steaming and baking, which enhance digestibility without sacrificing nutritional content. With these skills, you can craft meals that are both satisfying and beneficial for gastrointestinal health.
Cooking Techniques for Easier Digestion
In your gastroparesis diet, the choice of cooking methods can significantly impact how well your body tolerates various foods. Gentle cooking methods like steaming and pureeing can help **modify food texture**, making them easier to digest. Soups and stews made with **clear liquids** provide hydration and nourishment without added strain on your stomach. It’s also possible to use **gentle cooking methods** alongside **dietary adjustments** to enhance flavor while still prioritizing digestibility, leading to enjoyable meals while navigating challenges.
Creating High-Calorie Snacks
In the world of **snacks for gastroparesis**, finding high-calorie options can help you maintain your weight while ensuring you’re not overwhelming your digestive system with bulk. Nutrient-dense snacks such as nut butters spread on low-fiber crackers or **high-calorie meals** designed for individuals with motility disorders can be fantastic alternatives. Experimenting with **nutritional supplements** and incorporating **digestible carbohydrates** into your snacks will help you reach your caloric intake goals without adverse effects.
Sample Meal Ideas and Recipes for Gastroparesis
Incorporating a variety of **gastroparesis recipes** into your meal planning can keep it exciting and satisfying. Consider preparing smoothies with yogurt, banana, and peanut butter for breakfast or a soup base of pureed vegetables with shredded chicken for lunch. For dinners, opt for easy meals such as baked white fish served with mashed potatoes or fluffy scrambled eggs that are easy on your gastrointestinal system. Keep a **food diary** to track how your body reacts to new recipes and mark your favorites for future use.
Monitoring Symptoms and Making Adjustments
To optimize your gastronomes diet effectively, monitoring meal effects and adjusting accordingly is crucial. Keeping a **food diary** to log food intake and digestive responses can provide valuable insights that guide your nutrition and symptom management strategies. Additionally, consulting with a nutritionist for tailored advice on your diet can help indicate how to best manage **vitamin deficiencies** and ensure you’re meeting your body’s specific requirements.
Tracking Symptoms Through Diet
Utilizing a **food tracking for symptoms** approach will enable you to fine-tune your eating habits based on what works best for your body. This information can help you identify **food intolerances** and develop personalized dietary advice. Comparing this data with your symptom patterns can reveal triggers that worsen your condition, allowing for proactive adjustments to your **nutrition plan**. Continuous assessment helps maintain **digestive health** while navigating the complexities of gastroparesis.
Consultation and Support for Gastroparesis
Seek the support of dietary counseling and educational resources for gastroparesis, which will provide professional insights tailored to managing gastroparesis effectively. **Expert dietary advice** can prove invaluable as you navigate challenges, helping you maintain **electrolyte balance** and nutritional integrity within your eating patterns. Regular check-ins with a healthcare professional can help you stay informed about the latest recommendations and adapt your dietary strategy as needed.
Key Takeaways
- Opt for **low-fat**, **soft foods** that assist in digestion while adhering to **portion control**.
- Incorporate a variety of **easy-to-digest** meals and snacks into your diet for nutritional balance.
- Utilize **meal planning** and **cooking techniques** that promote better gut health.
- Monitor your symptoms regularly and consult with professionals for tailored dietary adjustments.
- Maintain hydration and consider nutrient supplementation as necessary to fill any gaps in your nutrition.
FAQ
1. What dietary supplements are recommended for gastroparesis?
Dietary supplements like protein shakes, vitamin D, and omega-3s can support those with gastroparesis by addressing potential **vitamin deficiencies** and improving overall nutrition. Consulting with a healthcare provider can help tailor supplementation to your specific needs.
2. How can I track my symptoms effectively?
Keeping a diligent **food diary** that includes what you eat, portion sizes, and any symptoms or reactions can help determine triggering foods or patterns. You can analyze this data to make informed adjustments to your **gastroparesis diet**.
3. What are examples of gentle cooking methods for gastroparesis?
Gentle cooking methods such as steaming, poaching, and baking preserve nutrients and yield easily digestible meals. These methods can help enhance flavor while ensuring that the food is well-tolerated for individuals with **gastroparesis**.
4. Should I avoid fiber entirely on a gastroparesis diet?
While it is advisable to limit high-fiber foods, including low-fiber options such as ripe bananas, comes can be beneficial. It’s best to consult a nutritionist to determine a suitable amount of **dietary fiber types** tailored to your needs.
5. What are some good snacks for people with gastroparesis?
Consider snacks like yogurt, low-fiber crackers with nut butter, or smoothies made with protein powder for an excellent source of calories and nutrition while remaining gentle on your stomach. Balanced **snack ideas for gastroparesis** can help maintain weight and energy levels.
### Images